Search
- Page Path
- HOME > Search
- Thyroid
- Prognostic Roles of Inflammatory Biomarkers in Radioiodine-Refractory Thyroid Cancer Treated with Lenvatinib
- Chae A Kim, Mijin Kim, Meihua Jin, Hee Kyung Kim, Min Ji Jeon, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Dong Yeob Shin, Won Gu Kim
- Endocrinol Metab. 2024;39(2):334-343. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1854
- 978 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
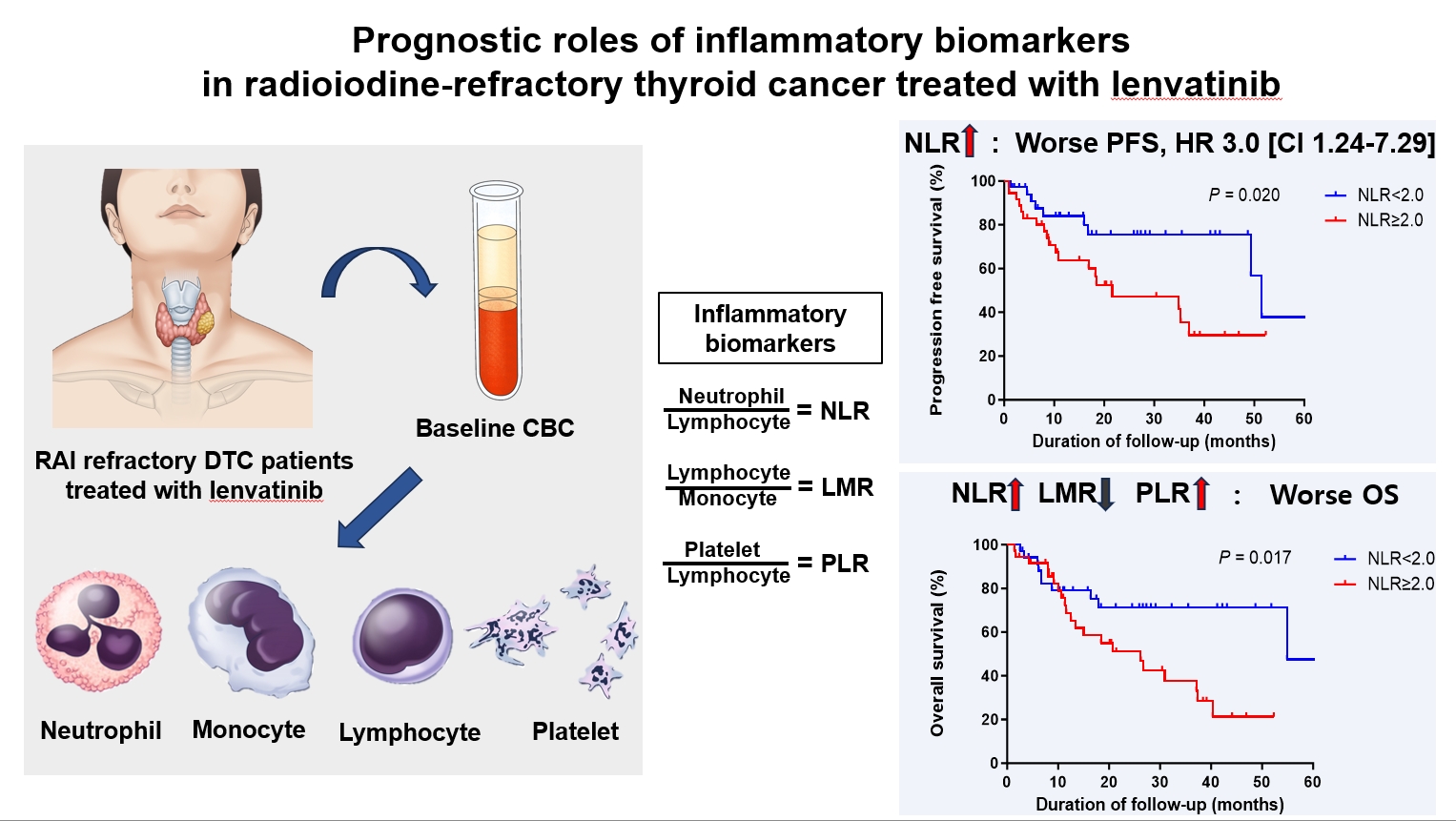
Inflammatory biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR), serve as valuable prognostic indicators in various cancers. This multicenter, retrospective cohort study assessed the treatment outcomes of lenvatinib in 71 patients with radioactive iodine (RAI)-refractory thyroid cancer, considering the baseline inflammatory biomarkers.
Methods
This study retrospectively included patients from five tertiary hospitals in Korea whose complete blood counts were available before lenvatinib treatment. Progression-free survival (PFS) and overall survival (OS) were evaluated based on the median value of inflammatory biomarkers.
Results
No significant differences in baseline characteristics were observed among patients grouped according to the inflammatory biomarkers, except for older patients with a higher-than-median NLR (≥2) compared to their counterparts with a lower NLR (P= 0.01). Patients with a higher-than-median NLR had significantly shorter PFS (P=0.02) and OS (P=0.017) than those with a lower NLR. In multivariate analysis, a higher-than-median NLR was significantly associated with poor OS (hazard ratio, 3.0; 95% confidence interval, 1.24 to 7.29; P=0.015). However, neither the LMR nor the PLR was associated with PFS. A higher-than-median LMR (≥3.9) was significantly associated with prolonged OS compared to a lower LMR (P=0.036). In contrast, a higher-than-median PLR (≥142.1) was associated with shorter OS compared to a lower PLR (P=0.039).
Conclusion
Baseline inflammatory biomarkers can serve as predictive indicators of PFS and OS in patients with RAI-refractory thyroid cancer treated with lenvatinib.

- Miscellaneous
- Corrigendum: Correction of Acknowledgments. Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2022;37(1):181-182. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.104
- Corrects: Endocrinol Metab 2021;36(2):359
- 2,822 View
- 110 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study
Sungho Bea, Heejun Son, Jae Hyun Bae, Sun Wook Cho, Ju‐Young Shin, Young Min Cho
Diabetes, Obesity and Metabolism.2024; 26(1): 108. CrossRef
- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study

- Clinical Study
- Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2021;36(2):359-364. Published online March 23, 2021
- DOI: https://doi.org/10.3803/EnM.2020.890
- Correction in: Endocrinol Metab 2022;37(1):181
- 5,824 View
- 202 Download
- 17 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
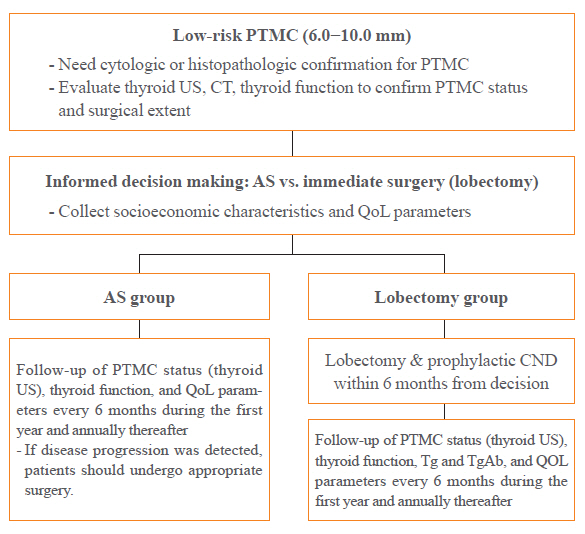
A Korean Multicenter Prospective cohort study of Active Surveillance or Surgery (KoMPASS) for papillary thyroid microcarcinomas (PTMCs) has been initiated. The aim is to compare clinical outcomes between active surveillance (AS) and an immediate lobectomy for low-risk PTMCs. We here outline the detailed protocol for this study.
Methods
Adult patients with a cytopathologically confirmed PTMC sized 6.0 to 10.0 mm by ultrasound (US) will be included. Patients will be excluded if they have a suspicious extra-thyroidal extension or metastasis of a PTMC or multiple thyroid nodules or other thyroid diseases which require a total thyroidectomy. Printed material describing the prognosis of PTMCs, and the pros and cons of each management option, will be provided to eligible patients to select their preferred intervention. For the AS group, thyroid US, thyroid function, and quality of life (QoL) parameters will be monitored every 6 months during the first year, and then annually thereafter. Disease progression will be defined as a ≥3 mm increase in maximal diameter of a PTMC, or the development of new thyroid cancers or metastases. If progression is detected, patients should undergo appropriate surgery. For the lobectomy group, a lobectomy with prophylactic central neck dissection will be done within 6 months. After initial surgery, thyroid US, thyroid function, serum thyroglobulin (Tg), anti-Tg antibody, and QoL parameters will be monitored every 6 months during the first year and annually thereafter. Disease progression will be defined in these cases as the development of new thyroid cancers or metastases.
Conclusion
KoMPASS findings will help to confirm the role of AS, and develop individualized management strategies, for low-risk PTMCs. -
Citations
Citations to this article as recorded by- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2024; 39(1): 47. CrossRef - It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Thyroid‐Stimulating Hormone, Age, and Tumor Size are Risk Factors for Progression During Active Surveillance of Low‐Risk Papillary Thyroid Microcarcinoma in Adults
Yasuhiro Ito, Akira Miyauchi, Makoto Fujishima, Takuya Noda, Tsutomu Sano, Takahiro Sasaki, Taketoshi Kishi, Tomohiko Nakamura
World Journal of Surgery.2023; 47(2): 392. CrossRef - Thyroid FNA cytology: The Eastern versus Western perspectives
Mitsuyoshi Hirokawa, Manon Auger, Chan Kwon Jung, Fabiano Mesquita Callegari
Cancer Cytopathology.2023; 131(7): 415. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - Long-Term Outcomes of Active Surveillance and Immediate Surgery for Adult Patients with Low-Risk Papillary Thyroid Microcarcinoma: 30-Year Experience
Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Akihiro Miya, Naoyoshi Onoda, Minoru Kihara, Takuya Higashiyama, Hiroo Masuoka, Shiori Kawano, Takahiro Sasaki, Mitsushige Nishikawa, Shuji Fukata, Takashi Akamizu, Mitsuru Ito, Eijun Nishihara, Mako Hisakad
Thyroid®.2023; 33(7): 817. CrossRef - Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status
Masashi Yamamoto, Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Takahiro Sasaki, Takumi Kudo
Thyroid®.2023; 33(10): 1182. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Optimal Cutoff Values of the Contact Angle of Tumor on Sonography System for Predicting Extrathyroidal Extension of Papillary Thyroid Carcinoma by Tumor Location
Ik Beom Shin, Do Hoon Koo, Dong Sik Bae
Clinical Medicine Insights: Oncology.2023;[Epub] CrossRef - Thermal ablation for papillary thyroid microcarcinoma located in the isthmus: a study with 3 years of follow-up
Lin Zheng, Fang-yi Liu, Jie Yu, Zhi-gang Cheng, Xiao-ling Yu, Xiao-cong Dong, Zhi-yu Han, Ping Liang
Future Oncology.2022; 18(4): 471. CrossRef - Trends in the Management of Localized Papillary Thyroid Carcinoma in the United States (2000–2018)
Elisa Pasqual, Julie Ann Sosa, Yingxi Chen, Sara J. Schonfeld, Amy Berrington de González, Cari M. Kitahara
Thyroid.2022; 32(4): 397. CrossRef - Management of Low-Risk Thyroid Cancers: Is Active Surveillance a Valid Option? A Systematic Review of the Literature
Renato Patrone, Nunzio Velotti, Stefania Masone, Alessandra Conzo, Luigi Flagiello, Chiara Cacciatore, Marco Filardo, Vincenza Granata, Francesco Izzo, Domenico Testa, Stefano Avenia, Alessandro Sanguinetti, Andrea Polistena, Giovanni Conzo
Journal of Clinical Medicine.2021; 10(16): 3569. CrossRef - Cost-Effectiveness Analysis of Active Surveillance Compared to Early Surgery in Small Papillary Thyroid Cancer: A Systemic Review
Han-sang Baek, Chai-ho Jeong, Jeonghoon Ha, Ja-Seong Bae, Jeong-soo Kim, Dong-Jun Lim, Chul-Min Kim
Cancer Management and Research.2021; Volume 13: 6721. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines

- Clinical Study
- Vandetanib for the Management of Advanced Medullary Thyroid Cancer: A Real-World Multicenter Experience
- Mijin Kim, Jee Hee Yoon, Jonghwa Ahn, Min Ji Jeon, Hee Kyung Kim, Dong Jun Lim, Ho-Cheol Kang, In Joo Kim, Young Kee Shong, Tae Yong Kim, Bo Hyun Kim
- Endocrinol Metab. 2020;35(3):587-594. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.687

- 5,670 View
- 147 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Vandetanib is the most widely used tyrosine kinase inhibitor for the treatment of patients with advanced medullary thyroid cancer (MTC). However, only limited data regarding its use outside clinical trials are available. We aimed to evaluate the efficacy and safety of vandetanib in patients with advanced MTC in routine clinical practice.
Methods
In this multicenter retrospective study, 12 patients with locally advanced or metastatic MTC treated with vandetanib at four tertiary hospitals were included. The primary outcome was the objective response rate (ORR) based on the Response Evaluation Criteria in Solid Tumors. The progression-free survival (PFS), overall survival (OS), and toxicities were also evaluated.
Results
Eleven patients (92%) had distant metastasis and 10 (83%) had disease progression at enrollment. Partial response was observed in five patients (ORR, 42%) and stable disease lasting ≥24 weeks was reported in an additional five patients (83%). During the median 31.7 months of follow-up, disease progression was seen in five patients (42%); of these, two died due to disease progression. The median PFS was 25.9 months, while the median OS was not reached. All patients experienced adverse events (AEs) which were generally consistent with the known safety profile of vandetanib. Vandetanib was discontinued in two patients due to skin toxicity.
Conclusion
Consistent with the phase III trial, this study confirmed the efficacy of vandetanib for advanced MTC in terms of both ORR and PFS in the real-world setting. Vandetanib was well tolerated in the majority of patients, and there were no fatal AEs. -
Citations
Citations to this article as recorded by- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance
Katerina Saltiki, George Simeakis, Olga Karapanou, Stavroula A. Paschou, Maria Alevizaki
Endocrine.2023; 80(3): 570. CrossRef - Initial Experiences of Selective RET Inhibitor Selpercatinib in Adults with Metastatic Differentiated Thyroid Carcinoma and Medullary Thyroid Carcinoma: Real-World Case Series in Korea
Han-Sang Baek, Jeonghoon Ha, Seunggyun Ha, Ja Seong Bae, Chan Kwon Jung, Dong-Jun Lim
Current Oncology.2023; 30(3): 3020. CrossRef - Molecular Basis and Natural History of Medullary Thyroid Cancer: It is (Almost) All in the RET
Nicolas Sahakian, Frédéric Castinetti, Pauline Romanet
Cancers.2023; 15(19): 4865. CrossRef - Sporadic Medullary Thyroid Carcinoma: Towards a Precision Medicine
Antonio Matrone, Carla Gambale, Alessandro Prete, Rossella Elisei
Frontiers in Endocrinology.2022;[Epub] CrossRef - Targeted therapy and drug resistance in thyroid cancer
Yujie Zhang, Zhichao Xing, Tianyou Liu, Minghai Tang, Li Mi, Jingqiang Zhu, Wenshuang Wu, Tao Wei
European Journal of Medicinal Chemistry.2022; 238: 114500. CrossRef - Daily Management of Patients on Multikinase Inhibitors’ Treatment
Carla Colombo, Simone De Leo, Matteo Trevisan, Noemi Giancola, Anna Scaltrito, Laura Fugazzola
Frontiers in Oncology.2022;[Epub] CrossRef - The Angiogenic Balance and Its Implications in Cancer and Cardiovascular Diseases: An Overview
Cătălina Ionescu, Bogdan Oprea, Georgeta Ciobanu, Milena Georgescu, Ramona Bică, Garofiţa-Olivia Mateescu, Fidan Huseynova, Veronique Barragan-Montero
Medicina.2022; 58(7): 903. CrossRef - Reassessing vascular endothelial growth factor (VEGF) in anti-angiogenic cancer therapy
Tobiloba C. Elebiyo, Damilare Rotimi, Ikponmwosa O. Evbuomwan, Rotdelmwa Filibus Maimako, Matthew Iyobhebhe, Oluwafemi Adeleke Ojo, Olarewaju M. Oluba, Oluyomi S. Adeyemi
Cancer Treatment and Research Communications.2022; 32: 100620. CrossRef - Current Guidelines for Management of Medullary Thyroid Carcinoma
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(3): 514. CrossRef - Recent advances in precision medicine for the treatment of medullary thyroid cancer
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Barbara Jarzab
Expert Review of Precision Medicine and Drug Development.2021; 6(5): 307. CrossRef - Functional evaluation of vandetanib metabolism by CYP3A4 variants and potential drug interactions in vitro
Mingming Han, Xiaodan Zhang, Zhize Ye, Jing Wang, Jianchang Qian, Guoxin Hu, Jianping Cai
Chemico-Biological Interactions.2021; 350: 109700. CrossRef - Nephrotoxicity in advanced thyroid cancer treated with tyrosine kinase inhibitors: An update
Alice Nervo, Francesca Retta, Alberto Ragni, Alessandro Piovesan, Alberto Mella, Luigi Biancone, Marco Manganaro, Marco Gallo, Emanuela Arvat
Critical Reviews in Oncology/Hematology.2021; 168: 103533. CrossRef
- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance

- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
- Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.272
- 9,516 View
- 429 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
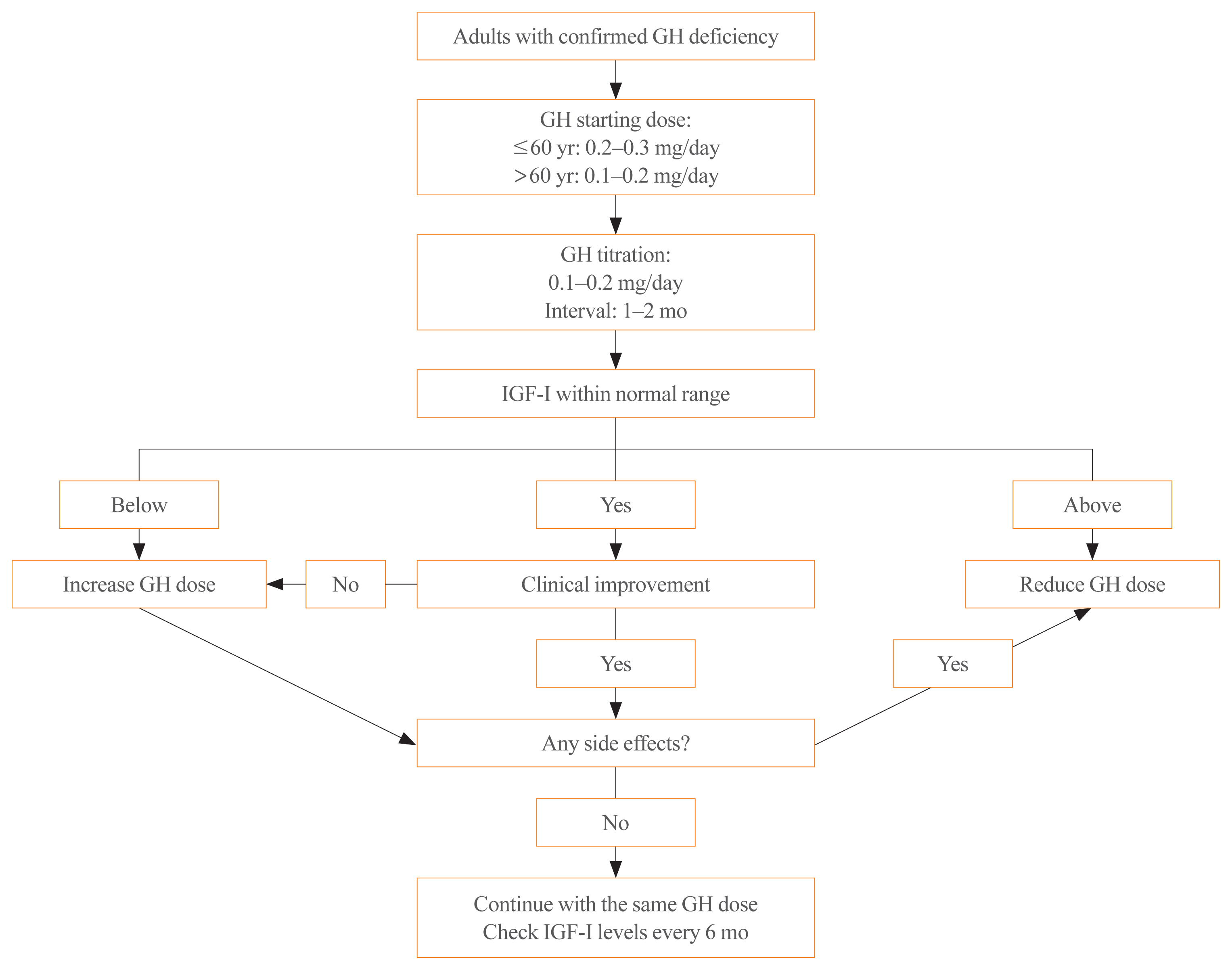
ePub - Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Efficacy, safety, and patient satisfaction of norditropin and sogroya in patients with growth hormone deficiency: a systematic review and meta-analysis of randomized controlled trials
Obieda Altobaishat, Mohamed Abouzid, Mostafa Hossam El Din Moawad, Abdulrahman Sharaf, Yazan Al-Ajlouni, Tungki Pratama Umar, Abdallah Bani-salameh, Mohammad Tanashat, Omar Abdullah Bataineh, Abdulqadir J. Nashwan
Endocrine.2024;[Epub] CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial

- Hypothalamus and Pituitary gland
- Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
- Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong Jun Lim, Dong Yeob Shin, Se Hwa Kim, Min Jeong Kwon, Ha Young Kim, Jin Hwa Kim, Dong Sun Kim, Chong Hwa Kim
- Endocrinol Metab. 2019;34(1):53-62. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.53
- 6,480 View
- 254 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub The Korean Endocrine Society (KES) published clinical practice guidelines for the treatment of acromegaly in 2011. Since then, the number of acromegaly cases, publications on studies addressing medical treatment of acromegaly, and demands for improvements in insurance coverage have been dramatically increasing. In 2017, the KES Committee of Health Insurance decided to publish a position statement regarding the use of somatostatin analogues in acromegaly. Accordingly, consensus opinions for the position statement were collected after intensive review of the relevant literature and discussions among experts affiliated with the KES, and the Korean Neuroendocrine Study Group. This position statement includes the characteristics, indications, dose, interval (including extended dose interval in case of lanreotide autogel), switching and preoperative use of somatostatin analogues in medical treatment of acromegaly. The recommended approach is based on the expert opinions in case of insufficient clinical evidence, and where discrepancies among the expert opinions were found, the experts voted to determine the recommended approach.
-
Citations
Citations to this article as recorded by- Hydrogel-fiber-mesh-based 3D cell cultures: A new method for studying pituitary tumors
Wooju Jeong, Sungrok Wang, Yumin Kim, Soohyun Lee, Minhu Huang, Jaeil Park, Myung-Han Yoon, Chang-Myung Oh, Cheol Ryong Ku
Smart Materials in Medicine.2024;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Growth Hormone Excess: Implications and Management
Suneela Dhaneshwar, Shrishti Shandily, Vatsalya Tiwari
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(6): 748. CrossRef - Revisiting the usefulness of the short acute octreotide test to predict treatment outcomes in acromegaly
Montserrat Marques-Pamies, Joan Gil, Elena Valassi, Marta Hernández, Betina Biagetti, Olga Giménez-Palop, Silvia Martínez, Cristina Carrato, Laura Pons, Rocío Villar-Taibo, Marta Araujo-Castro, Concepción Blanco, Inmaculada Simón, Andreu Simó-Servat, Gemm
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Octreotide in the treatment of acromegaly – the possibilities of high-dose therapy
I. A. Ilovayskaya
Meditsinskiy sovet = Medical Council.2022; (10): 148. CrossRef - Approach of Acromegaly during Pregnancy
Alexandru Dan Popescu, Mara Carsote, Ana Valea, Andreea Gabriela Nicola, Ionela Teodora Dascălu, Tiberiu Tircă, Jaqueline Abdul-Razzak, Mihaela Jana Țuculină
Diagnostics.2022; 12(11): 2669. CrossRef - Left to themselves: Time to target chronic pain in childhood rare diseases
Christine B. Sieberg, Alyssa Lebel, Erin Silliman, Scott Holmes, David Borsook, Igor Elman
Neuroscience & Biobehavioral Reviews.2021; 126: 276. CrossRef - Severe respiratory failure in a patient with COVID-19 and acromegaly: rapid improvement after adding octreotide
Jacob Luty, LesleAnn Hayward, Melanie Jackson, P Barton Duell
BMJ Case Reports.2021; 14(8): e243900. CrossRef - Precision Therapy in Acromegaly Caused by Pituitary Tumors: How Close Is It to Reality?
Cheol Ryong Ku, Vladimir Melnikov, Zhaoyun Zhang, Eun Jig Lee
Endocrinology and Metabolism.2020; 35(2): 206. CrossRef - Medical Treatment with Somatostatin Analogues in Acromegaly: Position Statement
Sang Ouk Chin, Cheol Ryong Ku, Byung Joon Kim, Sung-Woon Kim, Kyeong Hye Park, Kee Ho Song, Seungjoon Oh, Hyun Koo Yoon, Eun Jig Lee, Jung Min Lee, Jung Soo Lim, Jung Hee Kim, Kwang Joon Kim, Heung Yong Jin, Dae Jung Kim, Kyung Ae Lee, Seong-Su Moon, Dong
The Korean Journal of Medicine.2019; 94(6): 485. CrossRef
- Hydrogel-fiber-mesh-based 3D cell cultures: A new method for studying pituitary tumors

- Thyroid
- Response: Natural Course of Cytologically Benign Thyroid Nodules: Observation of Ultrasonographic Changes (Endocrinol Metab 2013;28:110-8, Dong Jun Lim et al.)
- Dong Jun Lim, Ki Hyun Baek
- Endocrinol Metab. 2013;28(3):243-244. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.243
- 2,825 View
- 23 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Calcification Patterns in Papillary Thyroid Carcinoma are Associated with Changes in Thyroid Hormones and Coronary Artery Calcification
Jeonghoon Ha, Jeongmin Lee, Kwanhoon Jo, Jeong-Sun Han, Min-Hee Kim, Chan Jung, Moo Kang, Bong Cha, Dong-Jun Lim
Journal of Clinical Medicine.2018; 7(8): 183. CrossRef
- Calcification Patterns in Papillary Thyroid Carcinoma are Associated with Changes in Thyroid Hormones and Coronary Artery Calcification

- Thyroid
- Natural Course of Cytologically Benign Thyroid Nodules: Observation of Ultrasonographic Changes
- Dong Jun Lim, Jee Young Kim, Ki Hyun Baek, Mee Kyoung Kim, Woo Chan Park, Jong Min Lee, Moo Il Kang, Bong Yun Cha
- Endocrinol Metab. 2013;28(2):110-118. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.110
- 4,292 View
- 37 Download
- 18 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The natural course of cytologically benign thyroid nodules remains unclear. The aim of this study was to evaluate whether ultrasonographic (US) changes are associated with changes in nodule volume during follow-up.
Methods We retrospectively reviewed over 4 years of clinical records of patients with benign thyroid nodules as confirmed by fine needle aspiration (FNA). In total, 186 patients with 202 benign thyroid nodules were included for study. We assessed for changes in nodule volume and examined the cystic portion of the nodule as well as four US features (echogenicity, margin, calcification pattern, and shape).
Results During follow-up (mean, 21.7±10.7 months) and using 50% as a cutoff value, nodule volumes increased in 11.8%, exhibited no change in 79.9%, and decreased in 8.3% of patients. Proportion of nodules demonstrating at least one US change was 20.8% (42/202). The most common US changes (in descending order of frequency) were cystic change, margin change, and calcification pattern change. Nodule shape and echogenicity rarely changed. Increased nodule volume was not significantly associated with any US features or with the number of FNAs but was associated with younger age at time of diagnosis.
Conclusion Although a portion of thyroid nodules confirmed as benign showed US changes or volume changes during the follow-up period, these findings may only represent the natural course of benign nodules. Frequent follow-up with US might be needed for only a small number of cases with suspicious US findings.
-
Citations
Citations to this article as recorded by- Follow-up of benign thyroid nodules confirmed by ultrasound-guided core needle biopsy after inconclusive cytology on fine-needle aspiration biopsy
Yoon Ji Hwang, Hye Ryoung Koo, Jeong Seon Park
Ultrasonography.2023; 42(1): 121. CrossRef - Clinical Characteristics, Diagnostic Approach and Outcome of Thyroid Incidental Findings vs. Clinically Overt Thyroid Nodules: An Observational Single-Centre Study
Tom Jansen, Nike Stikkelbroeck, Annenienke van de Ven, Ilse van Engen-van Grunsven, Marcel Janssen, Han Bonenkamp, Martin Gotthardt, Romana T. Netea-Maier
Cancers.2023; 15(8): 2350. CrossRef - Association between various thyroid gland diseases, TSH values and thyroid cancer: a case–control study
Leif Schiffmann, Karel Kostev, Matthias Kalder
Journal of Cancer Research and Clinical Oncology.2020; 146(11): 2989. CrossRef - TI-RADS und andere sonografische Klassifikationssysteme für Schilddrüsenknoten
Julian M. M. Rogasch, Christoph Wetz, Winfried Brenner
Onkologie up2date.2020; 2(03): 223. CrossRef - TI-RADS und andere sonografische Klassifikationssysteme für Schilddrüsenknoten
Julian M.M. Rogasch, Christoph Wetz, Winfried Brenner
Radiopraxis.2020; 13(01): E1. CrossRef - Changes of Nodular Size and Its Risk Factors in Iodine-Sufficient Area: a Retrospective Cohort Analysis of 7753 Thyroid Nodules
Hwa Young Ahn, Kyung Won Kim, Hoon Sung Choi, Jae Hoon Moon, Ka Hee Yi, Min Kyung Hyun, Min Joo Kang, Jung Im Shim, Ja Youn Lee, Do Joon Park, Young Joo Park
International Journal of Thyroidology.2020; 13(2): 118. CrossRef - Comparison of Natural Course between Thyroid Cancer Nodules and Thyroid Benign Nodules
Kyun-Jin Yun, Jeonghoon Ha, Min-Hee Kim, Ye Young Seo, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2019; 34(2): 195. CrossRef - Risk factors for hypothyroidism in euthyroid thyroid nodule patients with lymphocytic thyroiditis on fine needle aspiration cytology
Jeong-Min Lee, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Min-Hee Kim, Chan-Kwan Jung, So-Lyung Jung, Moo-Il Kang, Bong-Yun Cha, Dong-Jun Lim
The Korean Journal of Internal Medicine.2019; 34(6): 1287. CrossRef - Evaluation of the natural course of thyroid nodules in patients with acromegaly
Sema Ciftci Dogansen, Artur Salmaslioglu, Gulsah Yenidunya Yalin, Seher Tanrikulu, Sema Yarman
Pituitary.2019; 22(1): 29. CrossRef - TI-RADS und andere sonografische Klassifikationssystemefür Schilddrüsenknoten
Julian M.M. Rogasch, Christoph Wetz, Winfried Brenner
Der Nuklearmediziner.2019; 42(03): 206. CrossRef - Molecular profiling of thyroid nodule fine-needle aspiration cytology
Markus Eszlinger, Lorraine Lau, Sana Ghaznavi, Christopher Symonds, Shamir P. Chandarana, Moosa Khalil, Ralf Paschke
Nature Reviews Endocrinology.2017; 13(7): 415. CrossRef - Diagnostic accuracy of thyroid nodule growth to predict malignancy in thyroid nodules with benign cytology: systematic review and meta‐analysis
Naykky Singh Ospina, Spyridoula Maraka, Ana Espinosa DeYcaza, Derek O'Keeffe, Juan P. Brito, Michael R. Gionfriddo, M. Regina Castro, John C. Morris, Patricia Erwin, Victor M. Montori
Clinical Endocrinology.2016; 85(1): 122. CrossRef - Rapid thyroid nodule growth is not a marker for well-differentiated thyroid cancer
Claudius Falch, Steffen Axt, Bettina Scuffi, Alfred Koenigsrainer, Andreas Kirschniak, Sven Muller
World Journal of Surgical Oncology.2015;[Epub] CrossRef - Predicting the Size of Benign Thyroid Nodules and Analysis of Associated Factors That Affect Nodule Size
Seok Ho Seo, Tae Hyun Kim, Soon Ho Kim, Seung Hyun Lee, Jong Taek Kim, Dae Won Park, Dong Chul Lee
Chonnam Medical Journal.2015; 51(2): 97. CrossRef - Thyroid ultrasound findings in a follow-up survey of children from three Japanese prefectures: Aomori, Yamanashi and Nagasaki
Naomi Hayashida, Misa Imaizumi, Hiroki Shimura, Fumihiko Furuya, Noriyuki Okubo, Yasushi Asari, Takeshi Nigawara, Sanae Midorikawa, Kazuhiko Kotani, Shigeyuki Nakaji, Akira Ohtsuru, Takashi Akamizu, Masafumi Kitaoka, Shinichi Suzuki, Nobuyuki Taniguchi, S
Scientific Reports.2015;[Epub] CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Natural Course of Cytologically Diagnosed Benign Thyroid Nodules
Eun-Kyung Kim
Journal of Korean Thyroid Association.2014; 7(2): 136. CrossRef - Ruling in or ruling out thyroid malignancy by molecular diagnostics of thyroid nodules
Markus Eszlinger, László Hegedüs, Ralf Paschke
Best Practice & Research Clinical Endocrinology & Metabolism.2014; 28(4): 545. CrossRef - Insufficient Experience in Thyroid Fine-Needle Aspiration Leads to Misdiagnosis of Thyroid Cancer
Jung Il Son, Sang Youl Rhee, Jeong-taek Woo, Won Seo Park, Jong Kyu Byun, Yu-Jin Kim, Ja Min Byun, Sang Ouk Chin, Suk Chon, Seungjoon Oh, Sung Woon Kim, Young Seol Kim
Endocrinology and Metabolism.2014; 29(3): 293. CrossRef - Clinical Outcomes in Patients with Non-Diagnostic Thyroid Fine Needle Aspiration Cytology: Usefulness of the Thyroid Core Needle Biopsy
Sung Hak Lee, Min Hee Kim, Ja Seong Bae, Dong Jun Lim, So Lyung Jung, Chan Kwon Jung
Annals of Surgical Oncology.2014; 21(6): 1870. CrossRef - Letter: Natural Course of Cytologically Benign Thyroid Nodules: Observation of Ultrasonographic Changes (Endocrinol Metab 2013;28:110-8, Dong Jun Lim et al.)
Sun Wook Cho
Endocrinology and Metabolism.2013; 28(3): 241. CrossRef - Natural Course of Benign Thyroid Nodules
Kyung Won Kim
Endocrinology and Metabolism.2013; 28(2): 94. CrossRef - Response: Natural Course of Cytologically Benign Thyroid Nodules: Observation of Ultrasonographic Changes (Endocrinol Metab 2013;28:110-8, Dong Jun Lim et al.)
Dong Jun Lim, Ki Hyun Baek
Endocrinology and Metabolism.2013; 28(3): 243. CrossRef
- Follow-up of benign thyroid nodules confirmed by ultrasound-guided core needle biopsy after inconclusive cytology on fine-needle aspiration biopsy

- Pregnancy-induced Osteoporosis Combined with Multiple Compression Fractures: A Case Report.
- Ji Eun Lee, Jin Sun Jang, Sun Hee Ko, Min Hee Kim, Dong Jun Lim, Moo Il Kang, Bong Yun Cha, Sook Hee Hong, Ja seong Bae, Kyeoung Sik Ryu
- Endocrinol Metab. 2011;26(2):150-154. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.150
- 2,084 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pregnancy associated osteoporosis (PAO) is a rare condition. It may affect women during pregnancy or after the delivery and it can induce severe back pain. Physicians can find multiple compression fractures on the plain images of these patients. However, little is known about PAO, including the prevalence, the cause, the risk factors and the prognosis. Herein we report on a case of PAO in a 38-year-old female who suffered from severe back pain induced by multiple vertebral compression fractures. After excluding the possibility of unknown malignancy, the patient underwent vertebroplasty to improve the clinical symptom. The bone biopsy results confirmed multiple benign acute compression fractures. The patient was treated with oral bisphosphonate, calcium and vitamin D. She showed clinical improvement without developing any additional vertebral fracture. When young women during pregnancy or just after the delivery complain of persistent back pain, PAO should be considered in the differential diagnosis, and early recognition and treatment are needed for PAO.
-
Citations
Citations to this article as recorded by- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures
Eun Yeong Choe, Je Eun Song, Kyeong Hye Park, Hannah Seok, Eun Jig Lee, Sung-Kil Lim, Yumie Rhee
Journal of Bone and Mineral Metabolism.2012; 30(5): 596. CrossRef
- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures

- A Case of Pituitary Abscess that was Difficult to Diagnose due to Repeated Symptomatic Responses to Every Corticosteroid Administration.
- Jin Sun Jang, Jae Seung Yun, Jung Ah Shin, Min Hee Kim, Dong Jun Lim, Jae Hyung Cho, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Ho Young Son, Yong Kil Hong
- Endocrinol Metab. 2011;26(1):72-77. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.72
- 1,635 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Pituitary abscess is a rare pathology, but it is a potentially life-threatening condition. Therefore, timely intervention, including antibiotics and an operation, can prevent the morbidity and mortality in such cases. A 31-year-old woman, who was 16 months after her second delivery, presented with intermittent headache for 3 months. Amenorrhea, polyuria and polydipsia were noticed and the endocrinological hormone studies were compatible with panhypopituitarism and diabetes insipidus. Pituitary MRI demonstrated a 2.3 cm sized cystic mass with an upper small nodular lesion. Her symptoms such as headache and fever were repeatedly improved whenever corticosteroid was administered, which led us to suspect the diagnosis of an inflammatory condition like lymphocytic hypophysitis. During the hormone replacement therapy, her cystic pituitary mass had grown and her symptoms progressively worsened for another two months. The patient underwent trans-sphenoidal exploration and she turned out to have a pituitary abscess. At the 3-month follow-up, amenorrhea was noticed and her residual function of the pituitary was tested by a combined pituitary stimulation test. The results were compatible with panhypopituitarism. She received levothyroxine 100 microg, prednisolone 5 mg and desmopressin spray and she is being observed at the out-patient clinic. The authors experienced a patient with primary pituitary abscess that was confirmed pathologically and we report on its clinical course with a literature review.

- Central Diabetes Insipidus Surmised as from Post-obstructive Diuresis after Decompression Treatment for Neurogenic Bladder.
- Kang Woo Lee, Chul Woo Yang, Dong Jun Lim, Hyuk Sang Kwon, Mi Ja Kang, Eun Sook Kim, Kun Ho Yoon, Ho Young Son, Bong Yun Cha
- J Korean Endocr Soc. 2009;24(2):144-147. Published online June 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.2.144
- 2,114 View
- 25 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Post-obstructive diuresis after treatment for neurogenic bladder-induced obstructive kidney disease is a common symptom. As polyuria may develop in many other conditions as well, the present case is about a patient with a chief complaint of polyuria accompanied by nocturia, that was initially diagnosed as hydronephrosis due to the presence of neurogenic bladder and bladder dysfunction. The result of the water deprivation test, which was conducted for persistent diluted polyuria, yielded a final diagnosis of central diabetes insipidus, notwithstanding the strong impression of post-obstructive diuresis initially made because of a sudden increase in urine output after an indwelling catheter was inserted for bladder decompression.
-
Citations
Citations to this article as recorded by- A Case of Septo-Optic Dysplasia Resulting in Central Diabetes Insipidus and Nonobstructive Bilateral Hydronephrosis
Jong Hyun Kim, Kwang Bok Lee, Jeonghun Lee, Soo Min Nam, Kang-Woo Lee, Eu Gene Hwang, Geon Gil
Korean Journal of Medicine.2014; 87(2): 209. CrossRef
- A Case of Septo-Optic Dysplasia Resulting in Central Diabetes Insipidus and Nonobstructive Bilateral Hydronephrosis

- A Case of Graves' Disease Associated with Systemic Sclerosis.
- Yune Jeong Lee, Mee Kyoung Kim, Dong Jun Lim, Ki Hoon Hur, Ki Hyun Baek, Moo Il Kang, Chul Soo Cho, Kwang Woo Lee, Gyeong Sin Park
- J Korean Endocr Soc. 2007;22(3):220-224. Published online June 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.3.220
- 2,020 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Systemic sclerosis is associated with a broad spectrum of autoimmune thyroid diseases. The association between systemic scleroderma and hypothyroidism is well established. However, there have been very few reports concerning the association between hyperthyroidism and systemic scleroderma. We experienced a patient with Graves' disease who presented with muscle weakness and the patient was finally diagnosed with systemic sclerosis via pathological examination of the muscle. We describe here a rare case of systemic sclerosis associated with Graves` disease.
-
Citations
Citations to this article as recorded by- Systemic Sclerosis Associated with Non-small Cell Lung Cancer and Papillary Thyroid Cancer: Case Report and Literature Review
Ho Jae Kim, Jung Joo Kim, Hee Jung Park, Yong Tai Kim
The Korean Journal of Medicine.2017; 92(3): 316. CrossRef
- Systemic Sclerosis Associated with Non-small Cell Lung Cancer and Papillary Thyroid Cancer: Case Report and Literature Review


 KES
KES

 First
First Prev
Prev



